Changing your clinic management system is not just a technical move; it’s a strategic decision that affects revenue, patient experience and your team’s daily routine. Outdated medical software creates rework, errors and data loss that silently damage your results.
At the same time, many managers postpone this change because they fear downtime or losing data from the electronic health record. With good planning, however, you can migrate to a more modern clinic management software without disruption—and even use the change to redesign processes and increase productivity.
Why changing your system becomes necessary
In real life, almost no clinic wakes up “out of the blue” ready to switch systems. The decision usually comes from small, recurring issues that slowly turn into serious operational bottlenecks.
The most common reasons include:
- Slow access to patient data and clinical history.
- A rigid electronic health record that doesn’t fit each specialty.
- Lack of integration with billing, payments or online scheduling.
- Poor or slow support in critical moments.
- No regular updates for data security or regulations such as HIPAA.
When these factors show up often, the system stops being an ally and starts blocking the clinic’s growth.
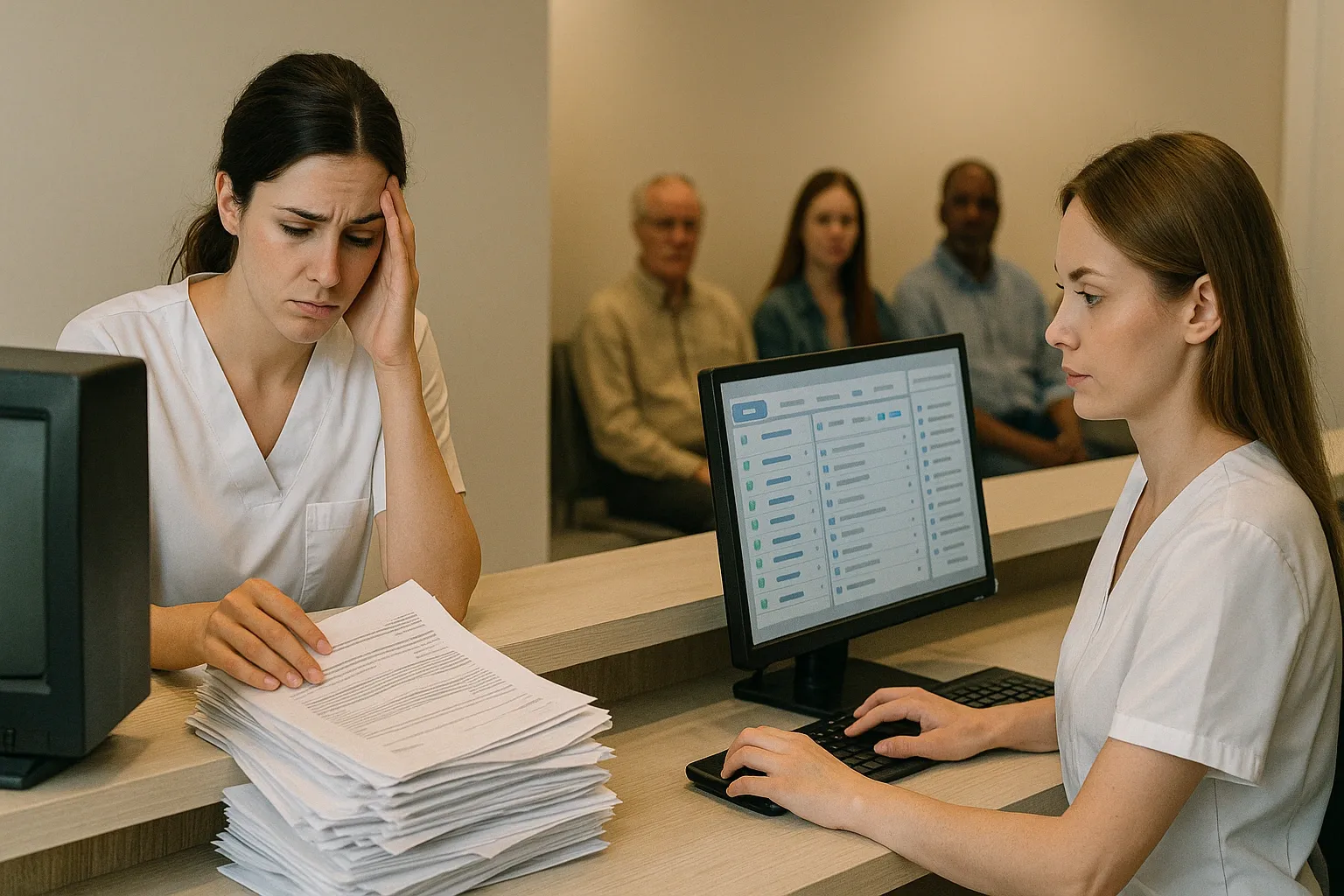
Signs that your medical software has become a bottleneck
Some very practical signs show that your current medical software is no longer keeping up with your operation:
- Front desk staff rely on extra spreadsheets to control add-ons, returns or waitlists.
- Physicians complain that the electronic health record is confusing, takes too many clicks and eats into consultation time.
- Leadership doesn’t have access to basic KPIs, such as revenue per unit, per provider or per line of service.
- The finance team does manual reconciliation because the clinic management system doesn’t integrate with payment platforms or practice management tools.
- Every new location requires “workarounds” to fit the existing management system.
If you recognize yourself in more than one of these points, it’s a strong sign that the system is delivering far less value than it should—and that change has become a strategic necessity.
Before we move on, one important note: if you manage a healthcare clinic and need better scheduling organization, a secure electronic health record, and centralized financial processes, Ninsaúde Clinic can streamline your daily operations. Get in touch to learn more.

Direct impact on patient experience
Patients may not know which clinic management software you use, but they definitely feel when operations are disorganized.
Long lines, constant delays, outdated contact data and communication failures (like missed appointment reminders) are often the result of a poorly configured or outdated clinic management system. This leads to frustration and increases the chance that the patient will look for another provider.
On the other hand, when your management system is well structured, the patient journey flows smoothly: easy scheduling, automatic confirmations, quick check-in, electronic health record accessed in a few clicks and agile document generation. That level of organization strengthens your brand and reinforces the value of your care.
Risks of staying on an outdated system
Postponing the switch to modern clinic management software carries a hidden cost that doesn’t show up as a single line in your P&L—but it affects profitability every day.
Key risks include:
- Data loss due to weak backup routines or old infrastructure.
- Legal and compliance risk, especially around how the electronic health record is stored and accessed.
- Limited scalability, because the system wasn’t built for multi-location or franchise operations.
Meanwhile, other clinics adopt modern medical software with automation and real-time dashboards, gaining a competitive edge both in care quality and in management.
How to assess if it’s time to switch systems
Before starting any migration, it’s worth making an honest assessment of your current situation. A few questions help guide this process:
- Does our clinic management system provide the KPIs leadership needs to make decisions?
- Does the electronic health record support the physician’s workflow—or get in the way?
- Can we integrate the medical software with other essential tools (labs, telehealth, billing, BI)?
- Is vendor support fast, reliable and specialized in healthcare?
If most answers are negative, you’re likely leaving money, efficiency and safety on the table—and a system change can generate a relatively quick return.

How to plan a migration without stopping the clinic
Switching a clinic management system requires care, but it doesn’t have to be chaotic. A solid migration plan typically follows a few steps.
1. Assign owners to the project
Choose an internal leader (manager, IT coordinator or operations director) and build a small committee with representatives from the front desk, clinical team and finance. This helps ensure the new clinic management software reflects how your operation actually works.
2. Map processes before you migrate
Before talking about features, you need to understand your current workflows: scheduling, add-ons and returns, clinical protocols, billing, follow-ups, recalls and reactivation campaigns.
This mapping guides how the new management system will be configured so it mirrors reality instead of forcing the team to adapt to a generic template.
3. Plan data migration from the electronic health record
Clinical and financial data are your most sensitive assets. Work with the new vendor to define how you’ll import patient records, visit history, documents, imaging and billing information.
Platforms like Ninsaúde Clinic provide specialized onboarding teams that guide each step of the process to reduce risk and ensure continuity of care during migration.
4. Run both systems in parallel for a period
In many cases, it’s smart to keep the old system available in read-only mode for a short period while the new clinic management system handles day-to-day operations.
This reduces anxiety for staff, gives physicians confidence to access older data if needed and avoids information gaps during the transition.
5. Invest in training and follow-up
Even the best medical software will fail if your team doesn’t know how to use it in real life.
Offer practical training tailored to each role—front desk, clinical staff, billing, management—and provide quick reference materials. Vendors like Ninsaúde Clinic typically offer close support during rollout, with channels such as chat, WhatsApp, phone and email, which shortens the learning curve.
What to look for in new clinic management software
When it’s time to choose your next system, you need to look beyond a checklist of basic features. Some differentiators make a big difference in daily operations:
- Flexible electronic health record, with customizable fields, templates and clinical protocols for each specialty.
- Smart scheduling, with automatic confirmations and the option for online booking.
- Robust financial tools, including integration with payment gateways and detailed management reports.
- Built-in patient communication, with reminders, recalls and segmented campaigns.
- Security and compliance, with audit trails, role-based access and adherence to regulations such as HIPAA.
Solutions like Ninsaúde Clinic stand out by integrating the electronic health record, scheduling, billing and CRM in a single clinic management system, reducing the need for spreadsheets and giving leadership a clearer view of the business.

Health franchises: extra challenges when switching systems
For health groups and franchise networks, changing medical software is even more sensitive, because it involves standardizing processes across locations while preserving local flexibility.
In these cases, the new clinic management system should:
- Support multiple locations with specific rules for pricing, schedules and teams.
- Provide consolidated dashboards by network, location and franchisee.
- Offer electronic health record templates that can be replicated and fine-tuned by specialty.
Clinic management software designed for franchises—such as Ninsaúde Clinic—helps maintain clinical and financial standards across the network while giving each site enough autonomy to run its day-to-day operations efficiently.
Switching systems is an investment in long-term sustainability
Switching your management system is not a “nice-to-have tech upgrade.” It’s a decision linked to operational efficiency, data security and patient experience.
When your medical software creates more problems than solutions, when the electronic health record slows down visits, when finance lives in isolated spreadsheets and leadership has no clear KPIs, it’s a sign that the time to change has arrived.
With solid planning, the right vendor and a strong focus on processes, migrating to a new clinic management system—such as Ninsaúde Clinic—can be the turning point toward a more organized, productive and sustainable phase for your clinic, group practice or healthcare franchise.
Enjoyed these insights?
Keep following our blog for more content on clinic management, medical marketing, and healthcare innovation.
Are you a healthcare professional who hasn’t tried Ninsaúde Clinic yet? Discover how the platform can streamline processes and elevate the quality of patient care.

