Telemedicine is no longer a temporary workaround—it’s a mature care delivery channel for visits, follow-ups, and patient retention. For practice owners, clinic managers, and physicians in private practice, the real differentiator isn’t just offering video visits. It’s embedding virtual care into a consistent, compliant clinical workflow. That’s where telemedicine integrated with the electronic health record (EHR) becomes essential: the visit happens inside the same environment where medical history, intake documentation, progress notes, clinical orders, and attachments live.
When telehealth and the EHR operate in separate systems, predictable problems follow: duplicated patient profiles, lost information, copy-and-paste charting, documents generated outside standardized workflows, and weak auditability. An EHR-integrated telemedicine workflow reduces friction and turns remote care into a seamless part of both clinical operations and patient experience.
Before we move on, one important note: if you manage a healthcare clinic and need better scheduling organization, a secure electronic health record, and centralized financial processes, Ninsaúde Clinic can streamline your daily operations. Get in touch to learn more.

What “telemedicine integrated with the EHR” means in practice
Telemedicine integrated with the EHR means the video visit is tied directly to the patient chart and encounter—without parallel steps. The clinician launches the visit from the schedule, opens the correct chart, reviews allergies, medications, prior notes, and results, and documents the encounter in real time. After the visit, clinical documentation, prescriptions, orders, and patient-facing instructions are associated with that same encounter, supporting traceability and continuity.
In practice, this creates a unified longitudinal record: in-person and virtual encounters become part of one timeline. For managers, it becomes easier to standardize documentation, monitor quality, and ensure chart completeness.
Clinical benefits: better continuity and safer decisions
The right context at the moment of decision
Telemedicine often involves fast-moving clinical scenarios: follow-ups, chronic care checks, medication adjustments, symptom triage, and lab review. If the clinician must jump across platforms to find key details, the risk of omissions rises. With an integrated EHR, decisions are supported by the patient’s real history—prior notes, problem lists, allergies, and relevant documents—available instantly.
Standardized intake templates and clinical protocols
An EHR-integrated telehealth workflow supports specialty-specific templates, structured forms, and checklists. That improves consistency, reduces variation across providers, and helps the practice deliver more uniform care—especially in multi-provider clinics where care continuity relies on reliable documentation.

Stronger chronic care and post-treatment follow-up
Telemedicine is particularly effective for chronic disease management, behavioral health, rehab check-ins, and post-op follow-ups. Integrated with the EHR, telehealth visits make it easier to track trends over time, compare results, document adherence, and update care plans quickly. Patients feel continuity, and practices gain predictable follow-up demand.
Operational benefits: less rework, more flow
Reduced front-desk burden and fewer loose ends
When telehealth is separate from the EHR, staff often create meeting links manually, send instructions via separate tools, and chase documentation afterward. With EHR-integrated telemedicine, the visit starts from scheduling and automatically connects to the correct chart and encounter—reducing repetitive tasks, lowering error risk, and improving operational speed.
Better schedule utilization and fewer no-shows
Integrated telehealth supports quick follow-ups and efficient visit types that keep schedules full without overloading the team. Pair this with automated reminders and confirmations, and practices often see fewer missed appointments and less inbound scheduling friction.

Physician productivity: fewer systems, faster documentation
An integrated workflow reduces tool switching and makes it easier to document during the visit. Prescriptions, visit summaries, referrals, and clinical instructions can be created while the patient is present—reducing after-hours charting and improving record quality.
Financial and strategic benefits
Scale care without expanding physical space
Virtual follow-ups and targeted telehealth visits can add capacity without requiring additional exam rooms. For managers, that means expanding visit volume while maintaining documentation standards. For clinicians, it can improve continuity and reduce cancellations caused by travel barriers. If billing workflows are integrated, practices can also improve revenue-cycle predictability by reducing administrative gaps between care and documentation.
Clearer performance visibility for data-driven management
When in-person and telehealth visits live in one EHR, operational metrics become more reliable. Telehealth volume, appointment adherence, visit cycle time, and follow-up frequency can be measured accurately. That supports smarter staffing, schedule design, and service mix decisions.
Better patient experience and higher retention
Patients don’t judge telehealth by video quality alone—they judge the whole journey: scheduling, reminders, the visit, and what happens afterward. When documentation and next steps are consistent and easy, trust increases. In healthcare, trust becomes retention and referrals.

Security and compliance in the U.S.: HIPAA-first telehealth
HIPAA-aligned privacy and security safeguards
Telemedicine involves protected health information (PHI), so compliance isn’t optional. An EHR-integrated telehealth workflow should support HIPAA-aligned safeguards such as access controls, authentication, encryption, audit logs, and role-based permissions. These measures reduce compliance exposure, support internal reviews, and strengthen governance.
Auditability and accountability
An integrated EHR provides a clear audit trail: who accessed the chart, who documented, when orders were created, and which documents were issued. This traceability supports quality initiatives, compliance readiness, and operational accountability—especially in multi-provider settings.
Interoperability and integrations
U.S. practices often rely on a broader ecosystem—billing tools, analytics, messaging, or specialty systems. Choosing a platform with strong integration capabilities (including APIs) reduces data silos and minimizes spreadsheet workarounds. Integration is what turns telehealth into a scalable, repeatable operational layer.
How to choose a telemedicine system with an integrated EHR (U.S. lens)
Confirm it’s truly integrated with scheduling and charting
The core requirement: launch the video visit from the schedule and chart directly inside the EHR—without duplicate logins, manual patient matching, or external links. If telehealth is just a separate tool, you’ll lose many of the efficiency gains.
Ensure in-visit clinical documentation and outputs
Verify you can generate clinically necessary outputs during the visit, such as e-prescriptions, visit summaries, referrals, and orders—within the same encounter and with proper documentation continuity.
Look for templates, structured forms, and efficiency features
Adoption follows ease of use. Specialty templates, customizable forms, and a clean longitudinal chart view make documentation faster and more consistent—improving both quality and operations.
Prioritize HIPAA-oriented security controls
Role-based access, audit logs, strong authentication options, encryption, and permission controls should be standard—especially for practices with multiple providers, locations, or support staff.
Evaluate the patient journey end-to-end
Online scheduling, automated reminders, pre-visit instructions, and a simple “join visit” flow reduce no-shows and elevate patient satisfaction. Telehealth success is as much about operational design as it is about video.
Ninsaúde Clinic as an example of EHR-integrated telemedicine
The best outcomes happen when telemedicine, the EHR, and clinic operations behave like one system—one schedule, one chart, one workflow. Ninsaúde Clinic is an example of a platform built around an integrated approach, bringing scheduling, the electronic health record, documentation, and structured forms into a unified workflow so telemedicine becomes part of the same clinical timeline as in-person care.
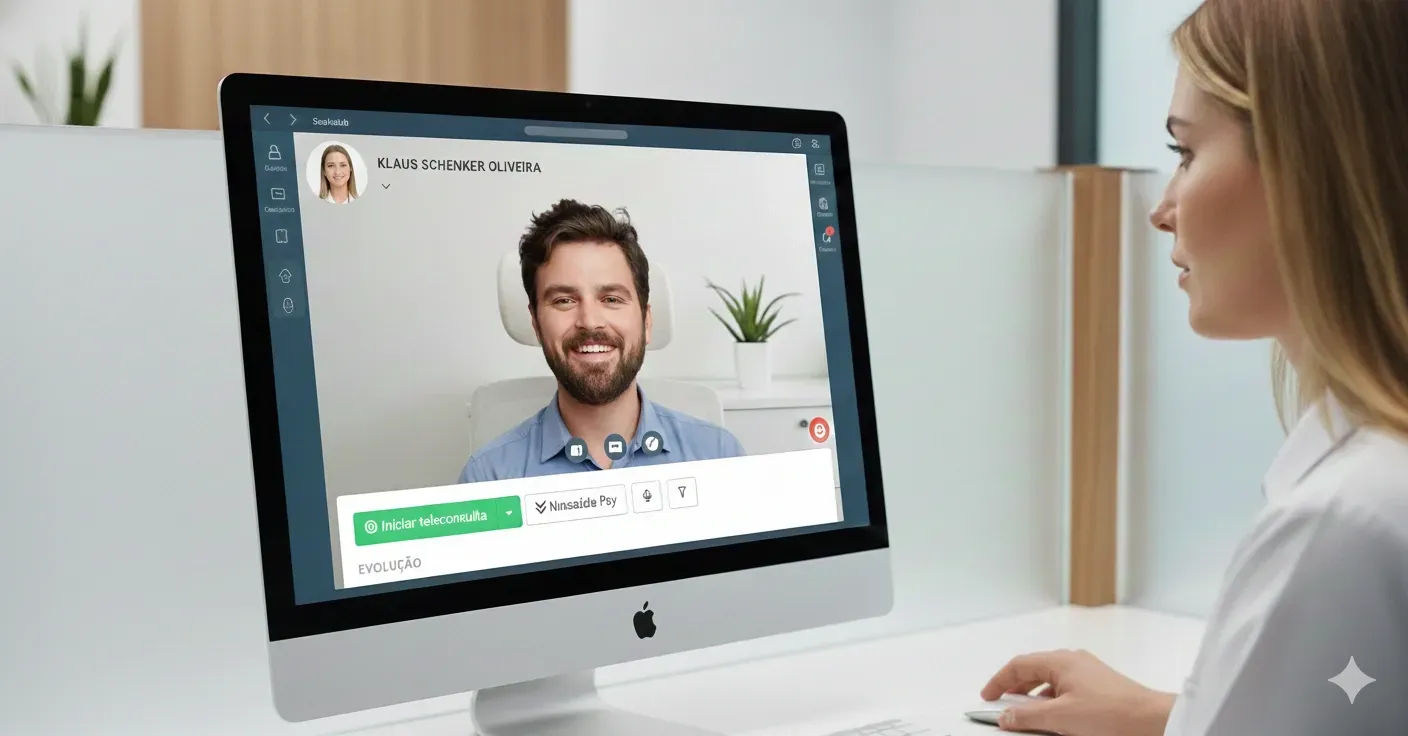
For managers, this kind of consolidation reduces tool sprawl, supports standardization, and improves auditability. For physicians, it speeds documentation, simplifies clinical outputs, and helps keep the patient record complete in one place.
Key takeaways to put into action
Telemedicine integrated with the electronic health record reduces rework, improves continuity of care, and strengthens documentation quality.
Scheduling-connected telehealth can reduce missed appointments and improve productivity for clinicians and staff.
Practices can scale care without expanding physical footprint while improving retention and operational visibility.
In the U.S., HIPAA-aligned safeguards—encryption, access controls, and audit logs—are foundational.
When selecting a system, prioritize true EHR integration, in-visit documentation outputs, standardization tools, and a frictionless patient journey.
Enjoyed these insights?
Keep following our blog for more content on clinic management, medical marketing, and healthcare innovation.
Are you a healthcare professional who hasn’t tried Ninsaúde Clinic yet? Discover how the platform can streamline processes and elevate the quality of patient care.

