The private healthcare ecosystem is under increasing pressure from rising costs, regulatory demands, and more discerning patients. In cardiology, where every minute matters, the difference between a good clinic and an excellent one appears in the operational details: no-show rates, wait times, room utilization, and the time between diagnosis and the start of treatment. Benchmarking in cardiology clinics organizes these details methodically, creating internal and market comparisons to guide decisions—not based on guesswork, but on data.
This practical guide shows, step-by-step, how to implement benchmarking in cardiology clinics: what to measure, how to collect data, how to compare, and most importantly, how to turn numbers into action plans that boost efficiency, quality, and revenue.
Before we continue, we need to ask: Are you already familiar with Ninsaúde Clinic? Ninsaúde Clinic is a medical software with an agile and complete schedule, electronic medical records with legal validity, teleconsultation, financial control and much more. Schedule a demonstration or try Ninsaúde Clinic right now!

What Benchmarking Is (Without the Buzzwords)
Benchmarking is the continuous process of comparing performance against internal and external references, understanding the reasons for a gap, and adopting superior practices. In cardiology clinics, this includes everything from triage and exam workflows (ECG, echocardiogram, ABPM, Holter, stress test) to patient service, billing, and treatment adherence.
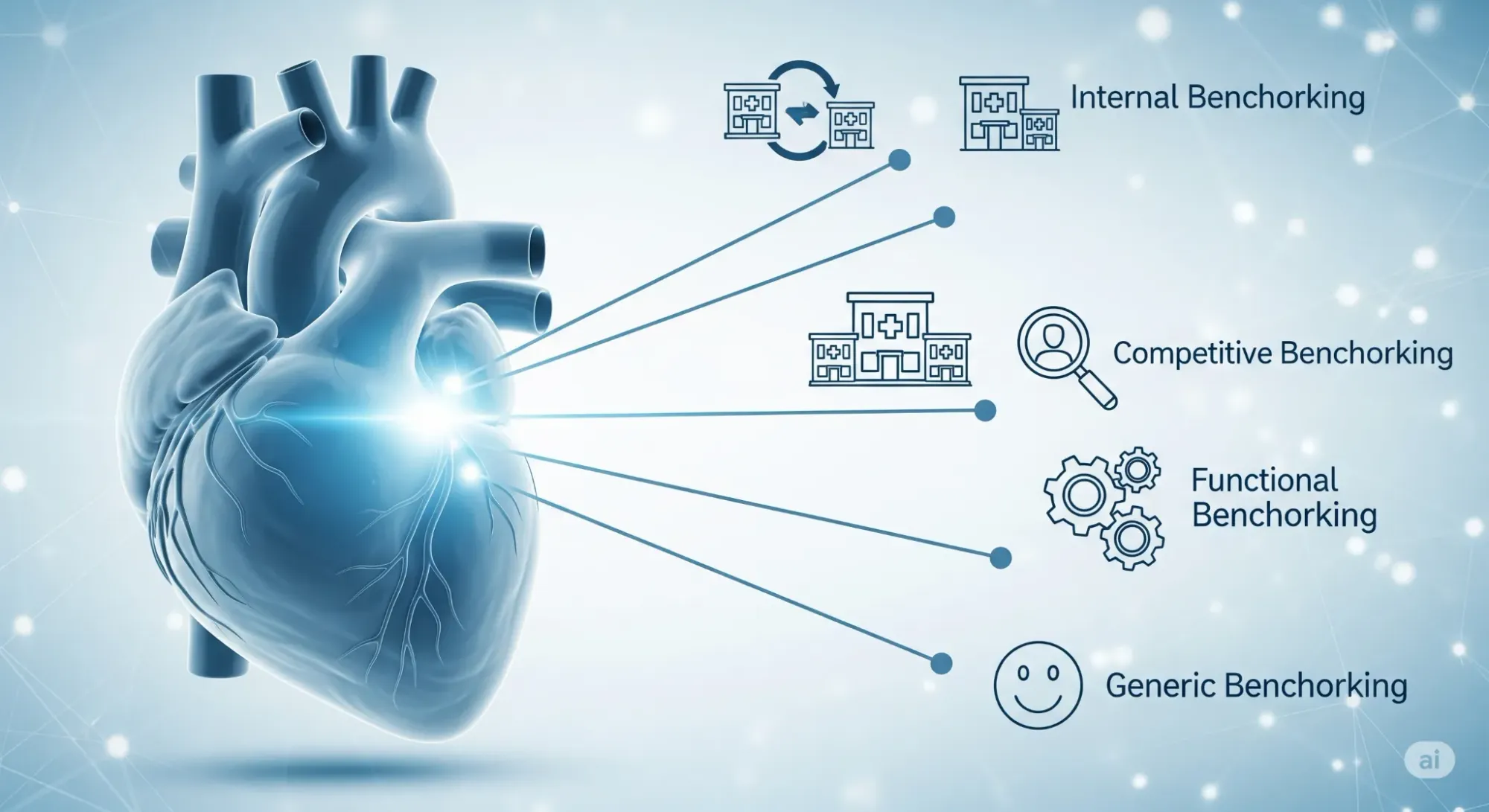
Four useful types:
- Internal: Compares units, teams, shifts, and rooms against each other.
- Competitive: Compares with similar clinics.
- Functional: Compares processes with high-efficiency sectors, even outside of cardiology.
- Generic: Compares universal indicators like NPS, absenteeism, and attendance rates.
Golden Rule: A benchmark without clinical context becomes just a spreadsheet of numbers. Always bring the cardiology reality to the table.
KPIs That Really Move the Needle in Cardiology
Avoid measuring "everything." Start with a lean set of indicators focused on access, quality, efficiency, and financial sustainability:
Access & Experience
- Average appointment time: from scheduling to checkout.
- No-show rate by service and health plan.
- NPS / CSAT post-consultation and post-exam.
Clinical Quality
- Time between clinical suspicion and completion of a key exam.
- % of patients with controlled blood pressure (BP) according to protocol.
- % of patients with LDL-C at target.
- Rate of unscheduled re-consultations within 30 days.
Operational Efficiency
- Schedule occupancy by room/equipment.
- Idle time and overcrowded shifts.
- Average report turnaround time.
- Front desk's AHT (Average Handle Time).
Financial & Growth
- Average ticket per service line.
- Billing and profitability profile (health plan/private pay mix and margin per procedure).
- Claim denials and time to payment.
- Lead conversion and attendance by channel.
💡 Tip: Stratify by risk/complexity for fair comparisons.
Data Sources and How to Standardize
Reliable data collection is half the battle. Combine:
- EHR and schedule for timings, occupancy, and resolution rates.
- Financial module for margins and revenue cycle.
- CRM/marketing for lead origins and conversion.
- Automated surveys for NPS/CSAT on Day+1.
Standardize measurement windows and create a data dictionary. Log workflow changes to maintain consistent historical comparisons.
Building the Benchmark: Internal, External, and "Aspirational"
- Internal Baseline (T0): 8–12 weeks of the clinic's own data.
- Internal Cross-Comparison: Between teams, shifts, rooms, and units.
- Prudent External Comparison: Cross-reference with benchmarks from associations, clinic groups, or consultants.
- Aspirational Benchmark: Goals based on the top quartile of the best-performing rooms/teams.
Visually, scorecards and radar charts help show "who is pulling ahead" and "who is holding back" the operation.

Translating Benchmarks into SMART Goals
A practical example:
- Problem: 18% no-show rate for ABPM; aspirational goal is ≤10%.
- Likely Cause: Late reminders and confusing instructions.
- SMART Goal: Reduce ABPM no-show rate to ≤10% within 90 days.
- Actions:
- Reminder + checklist via WhatsApp at T-72h/T-24h.
- Upfront payment for peak time slots.
- Controlled overbooking during critical windows.
- Counter-Metric: Patient satisfaction.
Operational Cycles: A Cadence That Keeps the Team in the Game
- Daily 10': Yesterday's indicators and today's bottlenecks.
- Weekly 30': Analysis of KPIs, root causes, and the plan for the week.
- Monthly 60': Review of goals, adjustment of levers, and budget.
Cardiology-Specific Best Practices
- Agenda organized by priority and follow-up: Dedicated slots for high-risk cases, clear return protocols, and follow-up for high-risk patients.
- Structured pre-consultation + coordinated exam workflow: Digital questionnaires to identify risks and optimize equipment setup times, preventing delays and increasing utilization.
Common Mistakes (and How to Avoid Them)
- Comparing without adjusting for complexity.
- Collecting too much data, analyzing too little.
- Goals without owners.
- Confusing an indicator with a diagnosis.
- Ignoring quality metrics as a counterbalance.
Mini Case Study
- Context: A clinic with two units, 12 consultation rooms, and 3 exam rooms.
- Baseline:
- Overall no-show rate: 14% (ABPM 23%).
- Average time to an echo: 12 days.
- Treadmill utilization: 61%, average setup time 12 min.
- Margin per exam: R$ 82; claim denials: 6.5%.
- Aspirational Benchmark:
- No-show rate: 9.5%.
- Time to an echo: 7 days.
- Treadmill utilization: 75%.
- Claim denials: 3.2%.
- 90-Day Plan:
- Escalated reminders + attendance guarantee.
- Quick checklist for treadmill setup.
- Pre-auditing of authorizations.
- Results:
- No-show rate: 10.2% (ABPM 11.4%).
- Time to an echo: 8 days.
- Treadmill utilization: 76%, setup time 7.5 min.
- Claim denials: 3.8%.

Tools and Automations That Shorten the Path
- Operational: Smart scheduling, digital check-in, WhatsApp confirmations, EHR with protocols, CRM for the patient journey.
- Strategic: Integrated financial software (denials, payment timelines, margins), dashboards, and APIs for BI.
Ninsaúde Clinic software integrates these modules, simplifying the consolidation of benchmarks by unit, room, and health plan—without fragile spreadsheets.
A Lean 30-60-90 Day Implementation Model
- 0–30 Days: Define scope, KPIs, and goals; set up automatic data capture; publish the initial scorecard.
- 31–60 Days: Execute priority actions and revise schedules according to demand.
- 61–90 Days: Standardize best practices and expand KPIs to clinical and financial areas.
Governance: Who Owns What
- Leadership: Defines global goals and budget; validates external benchmarks.
- Operations Manager: Ensures cadence and prioritization.
- Clinical Coordinators: Adapt goals to clinical routines.
- Front Desk/Contact Center: Own attendance and AHT.
- Billing: Owns claim denials and payment timelines.
- BI Analyst: Maintains data quality and visualizations.
Incentives: Connect bonuses and recognition to collective indicators, not just individual ones.
Compliance and Security
Consolidating data for benchmarking requires attention to data protection laws like GDPR or HIPAA. Work with anonymized or aggregated information, limiting access by role and maintaining activity logs.
Measures like encryption, secure backups, and access traceability prevent incidents and strengthen the clinic's reputation. Good compliance not only protects against legal risks but also increases the trust of patients and partners.
Quick Checklist
- [ ] KPIs defined and stratified by complexity and payer.
- [ ] Data dictionary and timeframes established.
- [ ] Automated data collection (schedule, EHR, financials, CRM).
- [ ] Scorecard with quartiles/medians.
- [ ] SMART goals with owners and counter-metrics.
- [ ] Meeting cadence: daily, weekly, monthly.
- [ ] Updated SOPs + training.
- [ ] Review of data protection policies and access profiles.
From Metrics to Excellence in Cardiology
Benchmarking is not a one-time project; it is a continuous management system. For cardiology clinics, it represents the chance to reduce wait times, improve the patient experience, optimize resources, and increase margins.
Start small with strategic indicators and gradually expand the analysis. Maintain discipline in data collection, security in data handling, and clarity in your goals—and with each cycle, your clinic will be one step closer to excellence.
Liked the information? Then prepare for a continuous journey of knowledge by following our blog. Are you a health professional and not yet familiar with the benefits of Ninsaúde Clinic? Stay ahead, optimize your processes, and elevate excellence in patient care!

